Nature Class - March 1997
(Page 2)
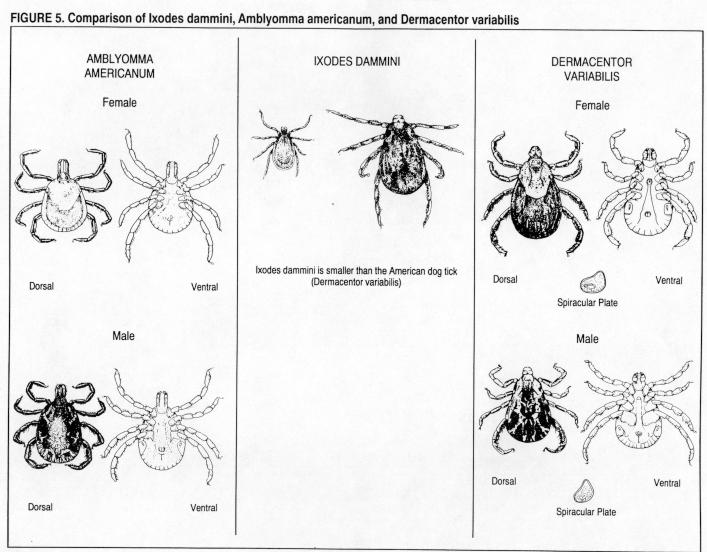
Recognizing the Tick
There are other hematophagous ticks in New Jersey, but they account for a very small percentage of the cases of LD. Mosquitoes typically take only one blood meal (although they can take more than one in their lifetime). It is unlikely that mosquitoes account for many cases of LD, since
B. burgdorferi seems not to survive within mosquitoes. Other ticks can be found in New Jersey, as well. The two that have been described are
Amblyomma americanum, known as the Lone Star tick, and Dermacentor
variabilis, known as the American or dog tick. Both of these are much larger than
Ixodes dammini and, as can be seen in Figure 5 (below), the appearance of the ticks is sufficiently different to allow differentiation between the ticks. This is important; only a very small percent of
Amblyomma americanum specimens have been found infected and only a very small number of cases can be attributed to its bite.
Dermacentor variabilis is probably so rarely infected that it is essentially never the vector responsible for LD.
Where can one expect to find the tick
Know areas of high risk: wooded areas, border areas, and brush.
Throughout its life cycle, the tick depends on mammalian hosts for meals. The most common hosts are mice and deer, although a variety of other animals can serve as hosts, as well. Therefore, areas where there are a lot of deer (you will not see the mice) are probably at risk; the sight of deer munching on your azaleas was once heartwarming, but no longer. However, we now know that LD occurs even in areas without deer; other medium to large-sized mammals substitute as the primary host for adult ticks. If your lawn is separated from the forest by only a little brush, then border between the forest and your property is a prime area for ticks, suspended on grass and shrubs, as noted above. (Modern developers have taken great pride in providing a natural environment and saving as much of the forest in their new properties as possible. By scalloping plots out of forest, they have maximized the very border niche preferred by ticks and mice and thereby have deposited new homeowners in an optimal environment for LD!!). If you want to walk in the woods, the most likely areas for tick residence would be the areas immediately adjoining deer paths. The deer "shed" ticks as they walk these paths, the eggs are laid, and the ticks live in this area; ticks do not wander very far and may never see much more than a few yards of the world unless carried elsewhere by a bird, dog, deer, or human.
Considering the above, it is obvious that a neat lawn in suburbia not near a forest is not a major risk area unless it is an area frequented by deer. In general, however, lawns are a hostile environment for ticks, as the ticks are more likely to dry out without shade and ground leaf clutter to protect them. A lawn in an urban area is also not an area of concern. It is the more rural areas which are at the most risk, and one can easily learn which areas are the hot spots of LD. Despite the figures, one cannot generalize about an entire county, any more than one can generalize about an entire state. There are areas of Ocean and Monmouth counties which represent centers of LD, but other areas which are relatively free of the disease. Local conditions will dictate this variation and it is worthwhile for the practitioner to keep track of changes in endemicity in her/his area of practice.
When is the tick active - "LD season"
From the previous description of the life cycle of Ixodes dammini it becomes clear that "LD season" is anytime there are hungry nymphs or adults out there. Thus, the major period for transmission is April through October, even though there may be many hungry ticks in your area well into the winter. In fact, if the weather in December or January permits people to go outside in the same clothes they might have worn in the fall, there may be new cases of LD during the winter. The reason for the end of "the season" is not that the ticks have left, but only that the average resident of New Jersey does not go out into the winter dressed in clothes which would allow a tick to get to the skin's surface. In northern California, where the weather is milder in the fall and winter,
new onset LD is reported during those periods and there is a flatter distribution of time of onset of the disease. Larvae, which are not infected, are found in greatest number between July and October, nymphs between April and August, and adults between October and May. Thus, there are potential risks of transmission in essentially any month of the calendar.
How long does the tick have to bite to transmit the infection?
There are no human studies of the required length of attachment of the tick prior to bite (would you volunteer to have an infected tick sit on your arm until it bit you?). Animal studies suggest that the tick spends 24 hours, even as long as 72 hours before completing its blood meal and transmitting B. burgdorferi. The tick takes a long time to embed its mouthparts and begin the feeding process. A precise figure for humans cannot be extrapolated from this, but recent retrospective studies on patients suggest that it is likely that transmission of LD takes about 48 hours.
What percentage of all tick bites can transmit the disease?
Recent studies have looked at what percentage of tick bites transmit LD. Studies done in areas where 20 to 40% of all adult ticks are infected have found that probably only 1% of all bites result in the transmission of the disease; in studies of prophylaxis for tick bites, the risk of an adverse reaction to the therapy is the same as the risk of acquiring the infection. One point to keep in mind: the individuals in these studies had identified the tick and removed it themselves. It is possible that these people removed the tick so soon after attachment that it did not have enough time to transfer B. burgdorferi (see previous
section).
Lack of evidence for other forms of transmission:
- Domestic animal to owner (cow, horse, dog)
- Casual or Intimate contact, sexual transmission
- Transfusion
- Transplacental transmission, breast milk
The recurring question from the public is "If the disease is only rarely spread by ticks other than
I. dammini, then what other means of transmission are there?". There has been much speculation about this, but as of this time there is no proof that LD can be spread directly from an animal to its owner; reports of transmission by infected urine have never been documented adequately. It is, of course, possible that your dog or cat could bring in a tick which had not yet attached and then pass it on to you. Certainly, dogs and cats can go places in the forest and shrubs most humans would not. Thus, they could be more at risk for picking up ticks. In fact, dogs can get LD. Most veterinarians in the state are on the lookout for LD in outdoor animals with arthritis or systemic disease. (As long as we are on the subject, there is a commercially available dog vaccine. Its safety and efficacy in dogs have recently been
proven in dogs, but it certainly has no place in the practice of human medicine.) Nonetheless, there is no accepted answer to the question of whether pet ownership represents a risk factor for developing LD, studies coming up with disparate results.
Casual or intimate contact, sexual or otherwise, is an unlikely means of transmission. It is far more likely that your spouse or sexual partner would pick up the infection from your mutually shared outdoor environment.
Published studies have demonstrated that B. burgdorferi in blood can survive the routine processing in blood banks, so that, theoretically, the organism could survive in the blood bank. We are unaware of any documented cases of LD being transmitted by transfusion. A recent study in Connecticut was unable to document any case of LD being transmitted in this manner.
Transplacental transmission of B. burgdorferi has been documented and cases of congenital LD have been reported. Transmission by breast milk has never been documented.
People at risk:
Children, Outside workers
Outside activities: Hunting, Camping, Hiking, Gardening
On the basis of the information above, one would predict that the people most at risk for getting LD would be those who spend the most time out of doors, in the "at-risk" environment, and this is true. Adventuresome and exploring children get LD more often than sedentary people. Twenty five percent of cases in New Jersey between 1978 and 1987 were children below the age of 10. Telephone linesmen, people involved in forestry or other maintenance work in endemic areas, as well as people whose hobbies involve being in such places, like hunters, campers, and hikers, are also at increased risk. If your gardening is done someplace where there are lots of deer or your vegetable patch is located next to brush or scrub on the verge of forest, you are also at risk.
Page 1
Page 2 |